J-Pouch
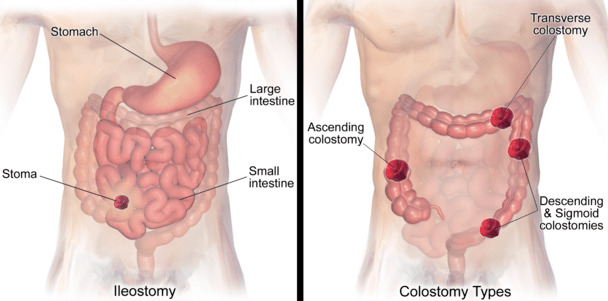
A J-Pouch is a common type of ostomy surgery. Some small intestine patients need a visible opening and bag on the outer wall of the abdomen; however, some need an internal pouch on the small intestine. The purpose of the internal and external pouches is the same both collect the stool. The creation of the j-pouch or an external stoma depends on the type of disease, the severity of the infection, patient’s requirements, patient’s age, overall physical condition, and other complexities in the digestive system.
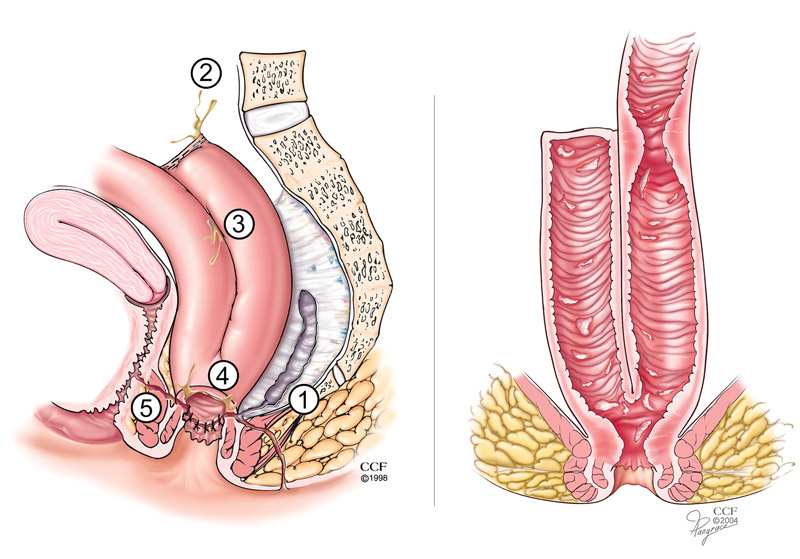
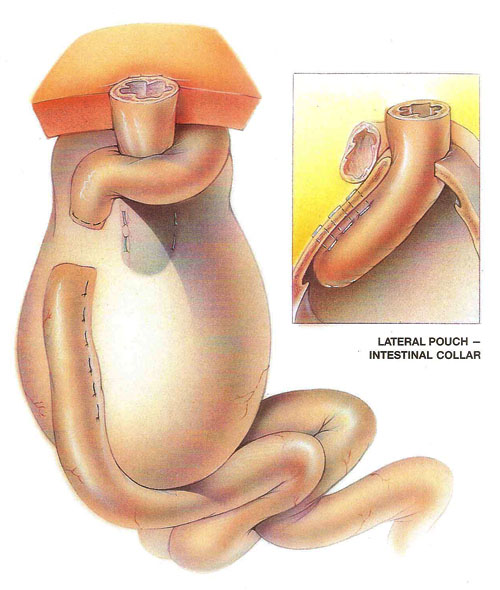
J-Pouch surgery is an alternative treatment of the ileostomy in a few cases. Sometimes, a patient wants a j-pouching operation instead of getting a stoma. However, doctors do not give an option all the time. A patient cannot select the j-pouch operation procedure in every disease. It can save a patient from getting an opening in the abdomen. It creates an internal bag to hold the stool. Thus, it is invisible and other people cannot see it. The procedure has two to three steps, depending on the patient’s condition. Usually, surgeons complete it in two stages only. The j-pouching surgery treats the ulcerative colitis and small intestine infections.
The j-pouch gives you some irritations and heaviness in your abdomen. Right after the j-pouching operation, a patient feels a change and discomfort in the digestive system, but this condition will not last forever. Once an ostomate gets used to the internal bag’s fulness, he/she can manage the situation, and of course, it will be a consoling situation than the pain and trouble you suffered from ulcerative colitis.
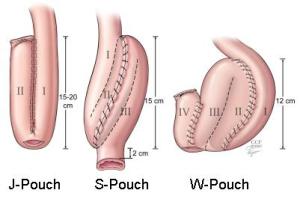
J-pouch surgery is not permanent. It only heals internal infections and ulcerative colitis. Doctors remove the internal sack once the disease gets eliminated from the digestive system. Moreover, the j-pouch appears on the small intestine or ileum, it comes in many shapes, including S, W, J. The appearance of the pouch depends on the internal condition and the looks of the ileum. This is a reversible procedure. An ostomate does not live the entire life with the j-pouch. Therefore, it requires more than one surgery. So, a patient should be young and healthy enough to bear and face two or three operations. Thus, this is usually an inappropriate incision for elderly people and the persons who have any other kind of disease, like heart disease, diabetes, cancer, brain tumor, arthritis, or any other physical problem.
Impacts of J-pouch on a Patient’s Life
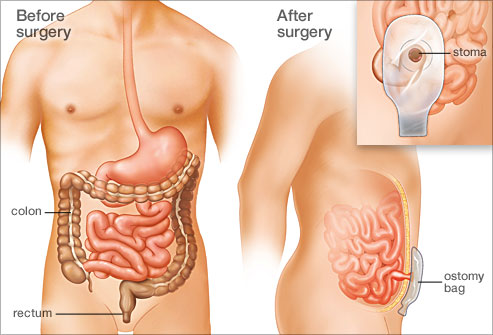
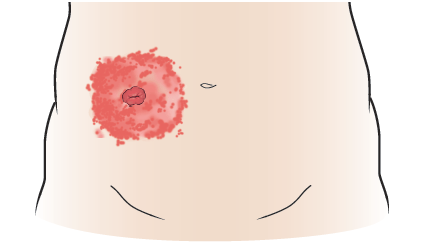
After the surgery, the pouching system changes the life of a person, but it does not take away normal things and lifestyle from you. The ostomy gives you a new organ in the abdomen and you need to take care of it. With time, changing, cleaning, and emptying the stoma, peristomal skin, and the pouching system become normal. A patient adapts the new routine. However, a jo-pouch operation does not bother you to change your appliances. As it does not discharge the stool from the stoma. It collects the feces in the internal j-pouch. Moreover, it ejects the waste through the anus. Thus, ostomates do not need to change the appliance routinely. However, when it comes to caring, you will have to take care of your diet and daily routine. Well, there is nothing harsh you need to do to look after your internal pouch. It will be the same as you do in stoma life. It takes time for healing ulcerative colitis. Once an ostomy patient gets rid of this disease, doctors remove the internal j-pouch and the patient can get back to the previous digestive system. Therefore, a patient can live a normal and happy life with the internal sack. It enhances the quality of spending life. Also, do not do anything physical without the permission of your ET nurse and doctor, like lifting weight, running, or hiking.